.
infection
[in-fek´shun]
invasion and multiplication of microorganisms in body tissues, as in an infectious disease. The infectious process is similar to a circular chain with each link representing one of the factors involved in the process. An infectious disease occurs only if each link is present and in proper sequence. These links are (1) the causative agent, which must be of sufficient number and virulence to destroy normal tissue; (2) reservoirs in which the organism can thrive and reproduce; for example, body tissues and the wastes of humans, animals, and insects, and contaminated food and water; (3) a portal through which the pathogen can leave the host, such as the respiratory tract or intestinal tract; (4) a mode of transfer, such as the hands, air currents, vectors, fomites, or other means by which the pathogens can be moved from one place or person to another; and (5) a portal of entry through which the pathogens can enter the body of (6) a susceptible host. Open wounds and the respiratory, intestinal, and reproductive tracts are examples of portals of entry. The host must be susceptible to the disease, not having any immunity to it, or lacking adequate resistance to overcome the invasion by the pathogens. The body responds to the invasion of causative organisms by the formation of
and by a series of physiologic changes known as
.
The spectrum of infectious agents changes with the passage of time and the introduction of drugs and chemicals designed to destroy them. The advent of antibiotics and the resultant development of resistant strains of bacteria have introduced new types of pathogens little known or not previously thought to be significantly dangerous to man. A few decades ago, gram-positive organisms were the most common infectious agents. Today the gram-negative microorganisms, and Proteus, Pseudomonas, and Serratia are particularly troublesome, especially in the development of hospital-acquired infections. It is predicted that in future decades other lesser known pathogens and new strains of bacteria and viruses will emerge as common causes of infections.
The development of resistant strains of pathogens can be limited by the judicious use of antibiotics. This requires culturing and sensitivity testing for a specific antibiotic to which the identified causative organism has been found to be sensitive. If the patient has been receiving a broad-spectrum antibiotic prior to culture and sensitivity testing, this should be discontinued as soon as the specific antibiotic for the organism has been found. It would be helpful, too, if the general public understood that antibiotics are not cure-alls and that there is danger in using them indiscriminately. In some instances an antibiotic can upset the normal flora of the body, thus compromising the body’s natural resistance and making it more susceptible to a second infection (superinfection) by a microorganism resistant to the antibiotic.
Although antibacterials have greatly reduced mortality and morbidity rates for many infectious diseases, the ultimate outcome of an infectious process depends on the effectiveness of the host’s immune responses. The antibacterial drugs provide a holding action, keeping the growth and reproduction of the infectious agent in check until the interaction between the organism and the immune bodies of the host can subdue the invaders.
Intracellular infectious agents include viruses, mycobacteria, Brucella, Salmonella, and many others. Infections of this type are overcome primarily by T lymphocytes and their products, which are the components of cell-mediated immunity. Extracellular infectious agents live outside the cell; these include species of Streptococcus and Haemophilus. These microorganisms have a carbohydrate capsule that acts as an antigen to stimulate the production of antibody, an essential component of humoral immunity.
Infection may be transmitted by direct contact, indirect contact, or vectors. Direct contact may be with body excreta such as urine, feces, or mucus, or with drainage from an open sore, ulcer, or wound. Indirect contact refers to transmission via inanimate objects such as bed linens, bedpans, drinking glasses, or eating utensils. Vectors are flies, mosquitoes, or other insects capable of harboring and spreading the infectious agent.Patient Care
. Major goals in the care of patients with threatening, suspected, or diagnosed infectious disease include the following: (1) prevent the spread of infection, (2) provide physiologic support to enhance the patient’s natural curative powers and resources for warding off or recovering from an infection, (3) provide psychologic support, and (4) prepare the patient for self-care if this is feasible.
Special precautions for prevention of the spread of infection can vary from strict isolation of the patient and such measures as wearing gloves, mask, or gown to simply using care when handling infective material. No matter what the diagnosis or status of the patient, handwashing before and after each contact is imperative.
Unrecognized or subclinical infections pose a threat because many infectious agents can be transmitted when symptoms are either mild or totally absent.
In the care of patients for whom special precautions have not been assigned, gloves are indicated whenever there is direct contact with blood, wound or lesion drainage, urine, stool, or oral secretions. Gowns are worn over the clothing whenever there is copious drainage and the possibility that one’s clothes could become soiled with infective material.
When a definitive diagnosis of an infectious disease has been made and special precautions are ordered, it is imperative that everyone having contact with the patient adhere to the rules. Family members and visitors will need instruction in the proper techniques and the reason they are necessary.
Physiologic support entails bolstering the patient’s external and internal defense mechanisms. Integrity of the skin is preserved. Daily bathing is avoided if it dries the skin and predisposes it to irritation and cracking. Gentle washing and thorough drying are necessary in areas where two skin surfaces touch, for example, in the groin and genital area, under heavy breasts, and in the axillae. Lotions and emollients are used not only to keep the skin soft but also to stimulate circulation. Measures are taken to prevent pressure ulcers from prolonged pressure and ischemia. Mouth care is given on a systematic basis to assure a healthy oral mucosa.
The total fluid intake should not be less than 2000 ml every 24 hours. Cellular dehydration can work against adequate transport of nutrients and elimination of wastes. Maintenance of an acid urine is important when urinary tract infections are likely as when the patient is immobilized or has an indwelling urinary catheter. This can be accomplished by administering vitamin C daily. Nutritional needs are met by whatever means necessary, and may require supplemental oral feedings or total parenteral nutrition. The patient will also need adequate rest and freedom from discomfort. This may necessitate teaching her or him relaxation techniques, planning for periods of uninterrupted rest, and proper use of noninvasive comfort measures, as well as judicious use of analgesic drugs.
Having an infectious disease can alter patients’ self-image, making them feel self-conscious about the stigma of being infectious or “dirty,” or making them feel guilty about the danger they could pose to others. Social isolation and loneliness are also potential problems for the patient with an infectious disease.
Patients also can become discouraged because some infections tend to recur or to involve other parts of the body if they are not effectively eradicated. It is important that they know about the nature of their illness, the purposes and results of diagnostic tests, and the expected effect of medications and treatments.
Patient education should also include information about the ways in which a particular infection can be transmitted, proper handwashing techniques, approved disinfectants to use at home, methods for handling and disposing of contaminated articles, and any other special precautions that are indicated. If patients are to continue taking antibacterials at home, they are cautioned not to stop taking any prescribed medication even if symptoms abate and they feel better.
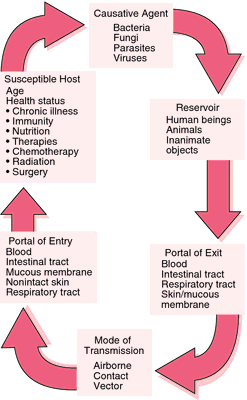
Chain of infection.
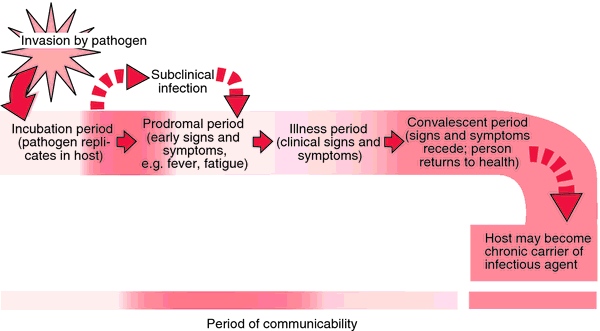
Stages of infection. Each period varies with different pathogens and different diseases.
airborne infection infection by inhalation of organisms suspended in air on water droplets or dust particles.
infection control 1.
in the
nursing interventions classification
, a
defined as minimizing the acquisition and transmission of infectious agents.
2.
the use of surveillance, investigation, and compilation of statistical data in order to reduce the spread of infection, particularly nosocomial infections.
Practitioners in infection control are often nurses employed by hospitals. They have titles such as Infection Control Officer and Infection Control Nurse, and they function as liaisons between staff nurses, physicians, department heads, the infection control committee, and the local health department. Such practitioners also assume some responsibility for teaching patients and their families, as well as employees of the hospital.
The centers for disease control and prevention is an excellent source of information related to infection control; their web site is http://www.cdc.gov. Another source of help and support for infection control practitioners is the Association for Practitioners in Infection Control and Epidemiology, 1275 K St., NW, Suite 100, Washington, DC 20005-4006.
cross infection infection transmitted between patients infected with different pathogenic microorganisms.
droplet infection infection due to inhalation of respiratory pathogens suspended on liquid particles exhaled by someone already infected.
dustborne infection infection by inhalation of pathogens that have become affixed to particles of dust.
endogenous infection that due to reactivation of organisms present in a dormant focus, as occurs, for example, in tuberculosis.
exogenous infection that caused by organisms not normally present in the body but which have gained entrance from the environment.
mixed infection infection with more than one kind of organism at the same time.
opportunistic infection
infection by an organism that does not ordinarily cause disease but becomes pathogenic under certain circumstances, as when the patient is
.
pyogenic infection infection by pus-producing organisms, most commonly species of Staphylococcus or Streptococcus.
risk for infection a nursing diagnosis accepted by the North American Nursing Diagnosis Association, defined as a state in which an individual is at increased risk for being invaded by pathogenic organisms.
secondary infection infection by a pathogen following an infection by a pathogen of another kind.
subclinical infection infection associated with no detectable symptoms but caused by microorganisms capable of producing easily recognizable diseases, such as poliomyelitis or mumps; this may occur in an early stage of the infection, with signs and symptoms appearing later during the course of the infection, or the symptoms and signs may never appear. It is detected by the production of antibody, or by delayed hypersensitivity exhibited in a skin test reaction to such antigens as tuberculoprotein.
terminal infection an acute infection occurring near the end of a disease and often causing death.
vector-borne infection infection caused by microorganisms transmitted from one host to another by a carrier, such as a mosquito, louse, fly, or tick.
waterborne infection infection by microorganisms transmitted in water.
in·fec·tion
(in-fek’shŭn),
Invasion of the body with organisms that have the potential to cause disease.
in·fec·tion
molysmophobia.
infection
/in·fec·tion/ (-fek´shun)
1. invasion and multiplication of microorganisms in body tissues, especially that causing local cellular injury due to competitive metabolism, toxins, intracellular replication, or antigen-antibody response.
2. an infectious disease.
airborne infection one that is contracted by inhalation of microorganisms or spores suspended in air on water droplets or dust particles.
droplet infection infection due to inhalation of respiratory pathogens suspended on liquid particles exhaled by someone already infected (droplet nuclei) .
endogenous infection that due to reactivation of organisms present in a dormant focus, as occurs in tuberculosis, etc.
tunnel infection subcutaneous infection of an artificial passage into the body that has been kept patent.
opportunistic infection infection by an organism that does not ordinarily cause disease but becomes pathogenic under certain circumstances (e.g., impaired immune responses).
infection
(ĭn-fĕk′shən)n.1.
a. The invasion of bodily tissue by pathogenic microorganisms that proliferate, resulting in tissue injury that can progress to disease: measures taken by the hospital to prevent infection.
b. The entry or placement, as by injection, of a microorganism or infectious agent into a cell or tissue.
c. An instance of being infected: developed an infection in my toe.
d. An agent or a contaminated substance responsible for one’s becoming infected: an infection spread by contaminated water.
e. The pathological state resulting from having been infected: a drug to control infection.
2. An infectious disease: Crowded conditions gave rise to several serious infections.
infection
[infek′shən]
Etymology: L, inficere, to stain
1 the invasion of the body by pathogenic microorganisms that reproduce and multiply, causing disease by local cellular injury, secretion of a toxin, or antigen-antibody reaction in the host.
2
a disease caused by the invasion of the body by pathogenic microorganisms. Compare
.
infectious, adj.
infection
Epidemiology The presence of a pathogen in a host which may or may not be associated with clinical disease. See Acute HIV infection, Atypical mycobacterial infection, Breakthrough infection, Chronic symptomatic HIV infection, Close contact infection, Congenital CMV infection, Cross-infection, Danger space infection, Ear infection, Emerging infection, Exit-site infection, Fungal infection, HIV-1 superinfection, Hyperinfection, Latent clostridial infection, Mixed wound infection, Multiple infection, Multiplicity of infection, Mycobacterial infection, Nail infection, Nonprogressive HIV infection, Nosocomial infection, Occult infection, Opportunistic infection, Parasitic infection, Perivascular inflammation, Ping pong infection, Pocket infection, Reemerging infection, Respiratory tract infection, Satellite infection, Silent infection, Spillover infection, Sterile infection, Subclinical infection, Superinfection, Surgical site infection, Tap water infection, Tunnel infection, Urinary tract infection. Cf Disinfection.
in·fec·tion
(in-fek’shŭn)
Invasion of the body by organisms that have the potential to cause disease.
infection
(in-fek’shon) [L. infectio, discoloration, dye]
A disease caused by microorganisms, esp. those that release toxins or invade body tissues. Worldwide, infectious diseases such as malaria, tuberculosis, hepatitis viruses, and diarrheal illnesses produce more disability and death than any other cause. Infection differs from colonization of the body by microorganisms in that during colonization, microbes reside harmlessly in the body or perform useful functions for it, e.g., bacteria in the gut that produce vitamin K. By contrast, infectious illnesses typically cause bodily harm.
Etiology
The most common pathogenic organisms are bacteria (including mycobacteria, mycoplasmas, spirochetes, chlamydiae, and rickettsiae), viruses, fungi, protozoa, and helminths. Life-threatening infectious disease usually occurs when immunity is weak or suppressed (such as during the first few months of life, in older or malnourished persons, in trauma or burn victims, in leukopenic patients, and in those with chronic illnesses such as diabetes mellitus, renal failure, cancer, asplenia, alcoholism, or heart, lung, or liver disease). Many disease-causing agents, however, may afflict vigorous persons, whether they are young or old, fit or weak. Some examples include sexually transmitted illnesses (such as herpes simplex or chlamydiosis), respiratory illnesses (influenza or varicella), and food or waterborne pathogens (cholera, schistosomiasis).
Symptoms
Systemic infections cause fevers, chills, sweats, malaise, and occasionally, headache, muscle and joint pains, or changes in mental status. Localized infections produce tissue redness, swelling, tenderness, heat, and loss of function.
Transmission
Pathogens can be transmitted to their hosts by many mechanisms, namely, inhalation, ingestion, injection or the bite of a vector, direct (skin-to-skin) contact, contact with blood or body fluids, fetomaternal contact, contact with contaminated articles (fomites), or self-inoculation.
In health care settings, infections are often transmitted to patients by the hands of professional staff or other employees. Hand hygiene before and after patient contact prevents many of these infections.
Defenses
The body’s defenses against infection begin with mechanisms that block entry of the organism into the skin or the respiratory, gastrointestinal, or genitourinary tract. These defenses include chemicals, e.g., lysozymes in tears, fatty acids in skin, gastric acid, and pancreatic enzymes in the bowel; mucus that traps the organism; clusters of antibody-producing B lymphocytes, e.g., tonsils, Peyer’s patches; and bacteria and fungi (normal flora) on the skin and mucosal surfaces that destroy more dangerous organisms. In patients receiving immunosuppressive drug therapy, the normal flora can become the source of opportunistic infections. Also, one organism can impair external defenses and permit another to enter; e.g., viruses can enhance bacterial invasion by damaging respiratory tract mucosa.
The body’s second line of defense is the nonspecific immune response, inflammation. The third major defensive system, the specific immune response, depends on lymphocyte activation, during which B and T cells recognize specific antigenic markers on the organism. B cells produce immunoglobulins (antibodies), and T cells orchestrate a multifaceted attack by cytotoxic cells. See: B cell; T cell; inflammation for table
Spread
Once pathogens have crossed cutaneous or mucosal barriers and gained entry into internal tissues, they may spread quickly along membranes such as the meninges, pleura, or peritoneum. Some pathogens produce enzymes that damage cell membranes, enabling them to move rapidly from cell to cell. Others enter the lymphatic channels; if they can overcome white blood cell defenses in the lymph nodes, they move into the bloodstream to multiply at other sites. This is frequently seen with pyogenic organisms, which create abscesses far from the initial entry site. Viruses or rickettsiae, which reproduce only inside cells, travel in the blood to cause systemic infections; viruses that damage a fetus during pregnancy (such as rubella and cytomegalovirus) travel via the blood.
Diagnosis
Although many infections (such as those that cause characteristic rashes) are diagnosed clinically, definitive identification of infection usually occurs in the laboratory. Carefully collected and cultured specimens of blood, urine, stool, sputum, or other body fluids are used to identify pathogens and their susceptibilities to treatment.
Treatment
Many infections, like the common cold, are self-limited and require no specific treatment. Understanding this concept is crucial because the misuse of antibiotics does not help the affected patient and may damage society by fostering antimicrobial resistance, e.g., in microorganisms such as methicillin-resistant Staphylococcus aureus. Many common infections, such as urinary tract infections or impetigo, respond well to antimicrobial drugs. Others, like abscesses, may require incision and drainage.
acute infection
An infection that appears suddenly and may be of brief or prolonged duration.
airborne infection
An infection caused by inhalation of pathogenic organisms in droplet nuclei.
apical infection
An infection located at the tip of the root of a tooth.
autochthonous infection
Infection caused by organisms normally present in the patient’s body. It may occur when host defenses are compromised, or when resident flora are introduced into an abnormal site.
bacterial infection
Any disease caused by bacteria. Bacteria exist in a variety of relationships with the human body. They colonize body surfaces and provide benefits, e.g., by limiting the growth of pathogens and by producing vitamins for absorption (in a symbiotic relationship). Bacteria can coexist with the human body without producing harmful or beneficial effects (in a commensal relationship). Bacteria may also invade tissues, damage cells, trigger systemic inflammatory responses, and release toxins (in a pathogenic or infectious relationship).
See: bacterium for table
bladder infection
blood-borne infection
An infection transmitted through contact with the blood (cells, serum, or plasma) of an infected individual. The contact may occur sexually, through injection, or via a medical or dental procedure in which a blood-contaminated instrument is inadvertently used after inadequate sterilization. Examples of blood-borne infections include hepatitis B and C and AIDS.
breakthrough infection
An infection that occurs despite previous vaccination.
chronic infection
An infection having a protracted course.
concurrent infection
The existence of two or more infections at the same time.
See: superinfection
cross infection
The transfer of an infectious organism or disease from one patient in a hospital to another.
cryptogenic infection
An infection whose source is unknown.
cytomegalovirus infection
Abbreviation: CMV infection
A persistent, latent infection of white blood cells caused by cytomegalovirus (CMV). Approx. 60% of people over 35 have been infected with CMV, usually during childhood or early adulthood; the incidence appears to be higher in those of low socioeconomic status. Primary infection is usually mild in people with normal immune function, but CMV can be reactivated and cause overt disease in pregnant women, AIDS patients, or those receiving immunosuppressive therapy following organ transplantation. CMV has been isolated from saliva, urine, semen, breast milk, feces, blood, and vaginal secretions of those infected; it is usually transmitted through contact with infected secretions that retain the virus for months to years.
During pregnancy, the woman can transmit the virus transplacentally to the fetus with devastating results. Approx. 10% of infected infants develop CMV inclusion disease, marked by anemia, thrombocytopenia, purpura, hepatosplenomegaly, microcephaly, and abnormal mental or motor development; more than 50% of these infants die. Most fetal infections occur when the mother is infected with CMV for the first time during this pregnancy, but they may also occur following reinfection or reactivation of the virus. Patients with AIDS or organ transplants may develop disseminated infection that causes retinitis, esophagitis, colitis, meningoencephalitis, pneumonitis, and inflammation of the renal tubules.
Etiology
CMV is transmitted from person to person by sexual activity, during pregnancy or delivery, during organ transplantation, or by contaminated secretions; rarely, (5%) blood transfusions contain latent CMV. Health care workers caring for infected newborns or immunosuppressed patients are at no greater risk for acquiring CMV infection than are those who care for other groups of patients (approx. 3%). Pregnant women and all health care workers should strictly adhere to standard infection control precautions.
Symptoms
Primary infection in the healthy is usually asymptomatic, but some people develop mononucleosis-type symptoms (fever, sore throat, swollen glands). Symptoms in immunosuppressed patients are related to the organ system infected by CMV and include blurred vision progressing to blindness; severe diarrhea; and cough, dyspnea, and hypoxemia. Antibodies seen in the blood identify infection but do not protect against reactivation of the virus.
Treatment
Antiviral agents such as ganciclovir and foscarnet are used to treat retinitis, colitis, and pneumonitis in immunosuppressed patients; chronic antiviral therapy has been used to suppress CMV, but this protocol has not been effective in preventing recurrence of CMV or development of meningoencephalitis. Ganciclovir has limited effect in congenital CMV. No vaccine is available.
Patient care
Health care providers can help prevent CMV infections by advising pregnant women and the immunocompromised to avoid exposure to contact with people who have confirmed and or suspected cases of CMV. The virus spreads from one person to another as a result of exposure to blood (as in transfusions) and other body fluids including feces, urine, and saliva. Contact with the diapers or drool of an infected child may result in infection of a person who has previously been unexposed to the infection. CMV is the most common congenital infection, affecting about 35,000 newborns each year. CMV infection that is newly acquired during the first trimester of pregnancy can be esp. hazardous to the developing fetus. As a result, young women who have no antibodies to CMV should avoid providing child care to infected youngsters. In the U.S., nurses who have failed to advise infected patients of the risk that CMV may pose to others have been judged to be negligent by the courts. Parents of children with severe congenital CMV require support and counseling. Although CMV infection in most nonpregnant adults is not harmful, it can cause serious illnesses or death in people with HIV/AIDS, organ transplants, and those who take immunosuppressive or cancer chemotherapeutic drugs. Infected immunosuppressed patients with CMV should be advised about the uses of prescribed drug therapies, the importance of completing the full course of therapy, and adverse effects to report for help in managing them. Family caregivers for infected people should be taught to observe standard precautions when handling body secretions. Since asymptomatic people may have and secrete the virus, standard precautions should be maintained by health care professionals at all times when such secretions are present or being handled.
deep neck infection
An infection that enters the fascial planes of the neck after originating in the oral cavity, pharynx, or a regional lymph node. It may be life-threatening if the infection enters the carotid sheath, the paravertebral spaces, or the mediastinum. Death may also result from sepsis, asphyxiation, or hemorrhage. Aggressive surgical therapy is usually required because antibiotics alone infrequently control the disease.
ULCER DUE TO DIABETIC FOOT INFECTION
diabetic foot infection
A polymicrobial infection of the bones and soft tissues of the lower extremities of patients with diabetes mellitus, typically those patients who have vascular insufficiency or neuropathic foot disease. Eradication of the infection may require prolonged courses of antibiotics, surgical débridement or amputation, or reconstruction or bypass of occluded arteries. Synonym:
See:
illustration
droplet infection
An infection acquired by the inhalation of a microorganism in the air, esp. one added to the air by sneezing or cough.
focal infection
Infection occurring near a focus, such as the cavity of a tooth.
fungal infection
Pathological invasion of the body by yeast or other fungi. Fungi are most likely to produce disease in patients whose immune defenses are compromised.
See: table
fungal infection of nail
Infection of a nail by one of a number of fungi. Systemic therapy with antifungal drugs may eradicate the infection.
health-care associated infection
Abbreviation: HAI
Nosocomial infection.
hospital-acquired infection
inapparent infection
An infection that is asymptomatic or is not detected.
local infection
An infection that has not spread but remains contained near the entry site.
low-grade infection
A loosely used term for a subacute or chronic infection with only mild inflammation and without pus formation.
nosocomial infection
An infection acquired in a hospital, nursing home, or other health care setting. Patients in burn units and surgical intensive care units have the highest rates of nosocomial infections. Synonym:
health-care associated infection
;
hospital-acquired infection
Patient care
Hospital-acquired infections result from the exposure of debilitated patients to the drug-altered environment of the hospital, where indwelling urinary catheters, intravenous lines, and endotracheal tubes enter normally sterile body sites and allow microbes to penetrate and multiply. Over 2 million nosocomial infections occur in the U.S. annually. Antibiotic-resistant organisms such as Enterobacter spp., Pseudomonas spp., staphylococci, enterococci, Clostridium difficile, and fungi often are responsible for the infectious outbreaks that result. Standard precautions and infection control procedures limit the incidence of nosocomial infections.
opportunistic infection
Abbreviation: OI
1. Any infection that results from a defective immune system that cannot defend against pathogens normally found in the environment. Common types include bacterial (Pseudomonas aeruginosa), fungal (Candida albicans), protozoan (Pneumocystis jirovecii), and viral (cytomegalovirus). Opportunistic infections are seen in patients with impaired defenses against disease, such as those with cystic fibrosis, poorly controlled diabetes mellitus, acquired or congenital immune deficiencies, or organ transplants.
2. An infection that results when resident flora proliferate and infect a body site in which they are normally present or at some other location. In healthy humans, the millions of bacteria in and on the body do not cause infection or disease. Host defenses and interaction with other microorganisms prevent excess growth of potential pathogens. A great number of factors, many poorly understood, may allow a normal bacterial resident to proliferate and cause disease.
pocket infection
Infection of the tissues beneath the skin into which an implanted device, such as a pacemaker or defibrillator, has been surgically inserted.
protozoal infection
An infection with a protozoon, e.g., malaria.
pyogenic infection
An infection resulting from pus-forming organisms.
reproductive tract infection
Abbreviation: RTI
Any infection of the reproductive organs. The most common causes are sexually transmitted diseases, but infections may also result from bacterial overgrowth or occasionally when instruments used in medical procedures introduce microorganisms. In women RTIs can cause pelvic pain, subfertility, infertility, or damage to the developing fetus. RTIs in men include epididymitis, prostatitis, and urethritis.
risk for infection
An immunocompromised state.
secondary infection
An infection made possible by a primary infection that lowers the host’s resistance, e.g., bacterial pneumonia following influenza.
slow virus infection
An infection caused by a virus that remains dormant in the body for a prolonged period before causing signs and symptoms of illness. Such viruses may require years to incubate before causing diseases. Examples include progressive multifocal leukoencephalopathy and subacute sclerosing panencephalitis.
subacute infection
An infection intermediate between acute and chronic.
subclinical infection
An infection that is immunologically confirmed but does not produce obvious symptoms or signs.
surgical site infection
An infection that occurs within thirty days of an operation, either at the suture line, just beneath it, or in internal organs and spaces that were operated upon.
Synonym: surgical wound infection
surgical wound infection
systemic infection
An infection in which the infecting agent or organisms circulate throughout the body.
terminal infection
An often fatal infection appearing in the late stage of another disease.
transfusion-associated bacterial infection
Transfusion-transmitted bacterial infection.
transfusion-transmitted bacterial infection
Abbreviation: TTBI.
Illness in a transfusion recipient that develops after the infusion of contaminated blood or blood products, esp. platelets. It usually results from colonization of the blood product during handling or storage or, less frequently, from an unsuspected infection in the blood donor. Coagulase-negative staphylococci are often responsible. Other bacteria that sometimes cause TTBI include Pseudomonas species, Anaplasma, Babesia, and Rickettsia.
Viruses may also be transmitted from blood donors to transfusion recipients. They may include cytomegalovirus, encephalitis viruses, and, rarely, hepatitis viruses or human immunodeficiency virus.
Synonym: transfusion-associated bacterial infection
upper respiratory infection
Abbreviation: URI
An imprecise term for any infection involving the nasal passages, pharynx, and bronchi. The cause is usually bacterial or viral, and, occasionally, fungal.
urinary tract infection
Abbreviation: UTI
Infection of the kidneys, ureters, or bladder by microorganisms that either ascend from the urethra (95% of cases) or that spread to the kidney from the bloodstream (5%). About 7 million Americans visit health care providers each year because of UTIs. These infections commonly occur in otherwise healthy women, men with prostatic hypertrophy or bladder outlet obstruction, children with congenital anatomical abnormalities of the urinary tract, and patients with urinary stasis related to incomplete bladder emptying, neurogenic bladder or indwelling bladder catheters. See:
;
;
;
Etiology
Escherichia coli causes about 80% of all UTIs. In young women, Staphylococcus saprophyticus is also common. In men with prostate disease, enterococci are often responsible. The small remaining percentage of infections may be caused by Klebsiella species, Proteus mirabilis, Staphylococcus aureus, Pseudomonas aeruginosa, or other virulent organisms.
Symptoms
The presenting symptoms of UTI vary enormously. Young patients with bladder infections may have pain with urination; urinary frequency or urgency, or both; pelvic or suprapubic discomfort; low-grade fevers; or a change in the appearance or odor of their urine (cloudy, malodorous, or rarely bloody). Older patients may present with fever, lethargy, confusion, delirium, or coma caused by urosepsis. Patients with pyelonephritis often complain of flank pain, prostration, nausea, vomiting, diarrhea, and high fevers with shaking chills. UTI may also be asymptomatic, esp. during pregnancy. Asymptomatic UTI during pregnancy is a contributing factor to maternal pyelonephritis, or fetal prematurity and stillbirth.
Diagnosis
Urinalysis (obtained either as a clean catch or catheterized specimen) and subsequent urinary culture are used to determine the presence of UTI, the suspect microorganism, and the optimal antibiotic therapy. A dipstick test may identify leukocyte esterase and nitrite in a urinary specimen, strongly suggesting a UTI. The presence of more than 8 to 10 white blood cells per high-power field of spun urine also strongly suggests UTI, as does the presence of bacteria in an uncentrifuged urinary specimen.
Treatment
Sulfa drugs, nitrofurantoin, cephalosporins, or quinolones may be used for the outpatient treatment of UTIs while the results of cultures are pending. Patients sick enough to be hospitalized may also be treated with intravenous aminoglycosides, medicine to treat nausea and vomiting, and hydration. The duration of therapy and the precise antibiotics used depend on the responsible organism and the underlying condition of the patient. Patients with anatomical abnormalities of the urinary tract, e.g., children with ureteropelvic obstruction or older men with bladder outlet obstruction, may sometimes require urological surgery.
Risk Factors
The following conditions predispose sexually active women to development of UTI: the use of a contraceptive diaphragm, the method of sexual intercourse, (greatly prolonged or cunnilingus), and failure to void immediately following intercourse.
Prevention of UTI in Young Women
Fluid intake should be increased to and maintained at to six to eight glasses daily. Although cranberry and other fruit juices are often recommended for patients with UTI, there is little objective evidence to show they have an impact. The urinary tract anesthetic phenazopyridine and sitz baths may provide relief from perineal discomfort. The anal area should be wiped from front to back or wipe the front first to prevent carrying bacteria to the urethral area; the bladder should be emptied shortly before and after intercourse; the genital area should be washed before intercourse; if vaginal dryness is a problem, water-soluble vaginal lubricants should be used before intercourse; a contraceptive diaphragm, cap, shield, or sponge should not remain in the vagina longer than necessary. An alternative method of contraception should be considered.
Patient care
Instructing the patient should emphasize self-care and prevention of recurrences. The antibiotic regimen should be explained, and the patient should be aware of signs and symptoms and, when they occur, should report them promptly to the primary caregiver.
yeast infection
A colloquial term for vulvovaginal candidiasis.
| Superficial Fungal Infections | |||
| Disease | Causative Organisms | Structures Infected | Microscopic Appearance |
| Epidermophytosis (e.g., dhobie itch) | Epidermophyton, (e.g., floccosum) | Inguinal, axillary, and interdigital folds; hairs not affected | Long, wavy, branched, and segmented hyphae and spindle-shaped cells in stratum corneum |
| Favus (tinea favosa) | Trichophyton schoenleinii | Epidermis around a hair; all parts of body; nails | Vertical hyphae and spores in epidermis; sinuous branching mycelium and chains in hairs |
| Ringworm (tinea, otomycosis) | Microsporum (e.g., audouinii) | Horny layer of epidermis and hairs, chiefly of scalp | Fine septate mycelium inside hairs and scales; spores in rows and mosaic plaques on hair surface |
| Trichophyton (e.g., tonsurans) | Hairs of scalp, beard, and other parts; nails | Mycelium of chained cubical elements and threads in and on hairs; often pigmented | |
| Thrush and other forms of candidiasis | Candida albicans | Tongue, mouth, throat, vagina, and skin | Yeastlike budding cells and oval thick-walled bodies in lesion |
| Systemic Fungal Infections | |||
| Aspergillosis | Aspergillus fumigatus | Lungs | Y-shaped branching of septate hyphae |
| Blastomycosis | Blastomyces brasiliensis, B. dermatitidis | Skin and lungs | Yeastlike cells demonstrated in lesion |
| Candidiasis | Candida albicans | Esophagus, lungs, peritoneum, mucous membranes | Small, thin-walled, ovoid cells |
| Coccidioidomycosis | Coccidioides immitis | Respiratory tract | Nonbudding spores containing many endospores, in sputum |
| Cryptococcosis | Cryptococcus neoformans | Meninges, lungs, bone, skin | Yeastlike fungus having gelatinous capsule; demonstrated in spinal fluid |
| Histoplasmosis | Histoplasma capsulatum | Lungs | Oval, budding, uninucleated cells |
infection
1. The process by which organisms capable of causing disease gain entry to the body and establish colonies.
2. The state of injury or damage to part of the body resulting from this process.
infection
the invasion of tissues by microorganisms with or without disease production.
infection
invasion and multiplication of microorganisms or parasites within tissue; signs of infection are masked in subclinical infection, or the immunocompromised; Table 1; see sepsis; Table 2
| Strategy | Examples of actions |
| Elimination of sources and reservoirs of infection | Care with exposure of infected lesions to avoid cross-contamination to adjacent tissues or the environment Use of appropriate disposable barrier clothing Decontamination of instruments following a recognized protocol Thorough hand-cleansing routines and the use of disposable gloves, especially if there are any cuts or infections on the clinician’s hands Avoiding patient contact if the clinician shows signs of infection Maintaining personal vaccination programmes Thorough cleaning of all parts of the clinical environment, appropriate disposal of clinical waste and elimination of chronically wet areas (such as soap dishes) |
| Disruption of routes of transmission | Frequent and regular decontamination of all: Hand-held equipment by scrubbing under running water or by immersion in an ultrasonic cleaning bath followed by exposure to pressurized steam by processing through an autoclave (immersion in disinfecting solutions and exposure to heat are no longer considered adequate) Large items of equipment by washing with water and detergent, drying then swabbing with alcohol wipes Meticulous hand-washing Use of elbow-operated liquid soap dispensers rather than bars of soap Use of single-use nail brushes Use of disposable paper towels Use of hypochlorite disinfectant solutions to clean up spillages of body fluids, according to the manufacturer’s instructions |
| Promoting host resistance | Preoperative preparation of the patient’s skin with chlorhexidine (0.5% chlorhexidine gluconate in 70% IMS) or povidone-iodine (10% povidone-iodine in water or IMS, releasing 1% active iodine), left in situ for 5 minutes Postoperative skin dressing of chlorhexidine or povidone-iodine Use of antimicrobial agents, such as silver, iodine, antibiotic or antifungal agents when frank infection is noted or suspected Advice to diabetic and immunocompromised patients on general care and health |
|
IMS, industrial methylated spirit. |
| Identified microorganism | Example of antimicrobial drug |
| Streptococci | Oral amoxicillin 500mg tds (or IV amoxicillin 500mg 8-hourly) |
| Staphylococci | Oral flucloxacillin 500mg qds (or IV flucloxacillin 500mg 6-hourly) |
| Anaerobes | Oral metronidazole 400mg tds (or IV metronidazole 500mg 8-hourly) |
| Gram-negatives | Oral ciprofloxacin 500mg bd (or IV ceftazidime 1g 6-hourly) |
|
IV, intravenous. |
infection
An invasion of the body by disease-producing microorganisms (e.g. bacteria, virus, fungus, parasite). Treatment typically includes anti-infective drugs, such as antibiotic, antifungal or antiviral agents.
Seeinflammation
.
in·fec·tion
(in-fek’shŭn)
Invasion of the body with organisms that have the potential to cause disease.
infection (infek´shən),
n an invasion of the tissues of the body by disease-producing microorganisms and the reaction of these tissues to the microorganisms and/or their toxins. The mere presence of microorganisms without reaction is not evidence of infection.
infection, adenovirus
,
n a proliferation of the adenovirus that may cause any number of illnesses, including “swimming pool conjunctivitis” and gastrointestinal or respiratory diseases, among others; it is possible to be infected without manifesting any symptoms.
infection, airborne
,
n an infection contracted by inhalation of microorganisms contained in air or water particles.
infection control
,
n procedures and protocols designed to prevent or limit cross-contamination in the health care delivery environment.
infection control, blood bank and blood transfusion
,
n.pl the precautions taken to ensure that blood-borne pathogens are not transmitted via donated blood; includes rejection of potential donors whose medical history shows evidence of viral hepatitis, drug addiction, or recent blood transfusions or tattoos, as well as laboratory testing of all donated blood for the presence of hepatitis B and C, syphilis, and the HIV-1 antibody.
infection control, surveillance
,
n the monitoring of the transmission of a disease in order to limit its occurrence.
infection, focal
,
n the process in which microorganisms located at a certain site, or focus, in the body are disseminated throughout the body to set up secondary sites, or foci, of infection in other tissues.
infection, hemolytic streptococcal
,
n 1. an infection usually caused by Group A hemolytic streptococci. Such infections include scarlet fever, streptococcal sore throat, cellulitis, and osteomyelitis.
2. an infection caused by streptococci that produce a toxic substance (hemolysin) that will lyse the erythrocytes and liberate hemoglobin from red blood cells.
infection, inflammatory
,
n an influx or accumulation of inflammatory elements (cellular and exudative) in the interstices of the tissues as a result of tissue injury by physical, chemical, microbiologic, and other irritants. Cellular elements include lymphocytes, plasma cells, polymorphonuclear leukocytes, and the macrophages of reticuloendothelial origin.
infection, latent
,
n a lingering infection that may lie dormant in the body for a time but may become active under certain conditions.
infection, local
,
n the prevention of excitation of the free nerve endings by literally flooding the immediate area with a local anesthetic solution.
infection, nosocomial
,
n an infection that first occurs during a patient’s stay at a health care facility, regardless of whether it is detected during the stay or after.
infection, opportunistic
,
n an illness or condition that occurs when pathogens are able to exploit a vulnerable host. An infection that is able to take hold because resistance is low.
infection, primary
,
n the original outbreak of an illness against which the body has had no opportunity to build antibodies; the originating infection.
infection, recurrent
,
n a reoccurrence of the same illness from which an individual has previously recovered.
infection, waterborne
,
n an illness that occurs as the result of drinking contaminated water or of eating fish that has been taken from contaminated waters.
infection
1. invasion and multiplication of microorganisms in body tissues, especially that causing local cellular injury due to competitive metabolism, toxins, intracellular replication or antigen-antibody response.
2. an infectious disease.
acute infection
short duration, of the order of several days.
airborne infection
infection by inhalation of organisms suspended in air on water droplets or dust particles.
arrested infection
restrained in its development by a capsule or adhesion but still containing infective material.
chronic infection
long duration, of the order of weeks or months.
infection control
the utilization of procedures and techniques in the surveillance, investigation and compilation of statistical data in order to reduce the spread of infection, particularly nosocomial infections.
cross infection
infection transmitted between patients infected with different pathogenic microorganisms.
droplet infection
infection due to inhalation of respiratory pathogens suspended on liquid particles exhaled by an animal that is already infected.
dustborne infection
infection by inhalation of pathogens that have become affixed to particles of dust.
endogenous infection
that due to reactivation of organisms present in a dormant focus, as occurs in tuberculosis, etc.
exogenous infection
that caused by organisms not normally present in the body but which have gained entrance from the environment.
general infection
see systemic infection (below).
latent infection
the animal is infected but there are no clinical signs nor infectious agent detectable in discharges.
local infection
has a common syndrome of varying degree, depending on the site and acuteness of the lesion and the type of microorganisms present, including fever, toxemia and leukocytosis with a left shift. The specific individual signs relate to the location of the lesion and the pressure it exerts on nearby organs. See also
,
,
,
,
,
,
,
,
,
.
masked infection
an infection is known to occur but the infectious agent cannot be demonstrated, e.g. the sheep-associated
catarrhal fever virus.
mixed infection
infection with more than one kind of organism at the same time.
nosocomial infection
pertaining to or acquired in hospital.
opportunistic infection
infection with organisms which are normally harmless but become pathogenic when the body’s defense mechanisms are compromised.
patent infection
one in which the infectious agent can be demonstrated in discharges of the patient.
persistent infection
a characteristic of some viruses, particularly herpesviruses and lentiviruses, in which there may be long-lasting or life-long latent infections, with asymptomatic periods and recurring acute episodes of clinical disease (herpesviruses) or onset of severe clinical disease (lentiviruses).
pyogenic infection
infection by pus-producing organisms.
secondary infection
infection by a pathogen following an infection by a pathogen of another kind.
subclinical infection
infection associated with no detectable signs but caused by microorganisms capable of producing easily recognizable diseases, such as mastitis or brucellosis; often detected by the production of antibody, or by delayed hypersensitivity exhibited in a skin test reaction to such antigens as tuberculoprotein.
super infection
a second infection occurs in an animal which is already experiencing an infection with another agent.
systemic infection
the infection is widespread throughout the body and must be assumed to be in all organs.
terminal infection
an acute infection occurring near the end of a disease and often causing death.
transmissible infection
an infection capable of being transmitted from one animal to another. Called also contagious.
waterborne infection
infection by microorganisms transmitted in water.
Patient discussion about infection
Q. Yeast infection in bloodstream How to get rid of yeast infection systemically.
A. there are several treatments and medications against systemic fungal infections, yeasts included. but in order to get treated you have to go through a proper diagnosis and a Dr. should check what kind of fungus you are having and prescribe the medication that fits it. me throwing all sort of medication names won’t give you anything. this has to be checked out with a blood test and a culture.
Q. Is this an infection or pregnancy? I am worried with the white odorless mucus discharge. My hubby and I are also trying for baby. I have browsed the web and found that this could be possible infection also. Is this an infection or pregnancy?
A. It’s a cervical discharge and mucus secreted may be majorly a sign of pregnancy. I too had the same symptom but was tested positive for pregnancy. At times it may be a normal vaginal discharge. Generally it will be a yeast infection. Just check for your body temperature changes as it indicates good for you. Your mucus will be like raw egg white, the more thick more chances for positive. Keep a check on these factors. I shall suggest you to visit the doctor to confirm the same instead of making your own conclusions.
Q. What are the symptoms of salmonella infection?
A. Dehydration is the principal clinical concern. The incubation period – the time between ingestion of Salmonella bacteria and the onset of illness – varies from six to 72 hours.Salmonella can cause three different kinds of illness: gastroenteritis, typhoid fever, and bacteremia.Symptoms of Salmonella gastroenteritis include diarrhea, abdominal cramps, fever, nausea, and/or vomiting.In mild cases diarrhea may be non-bloody, occur several times per day, and not be very voluminous; in severe cases it may be frequent, bloody and/or mucoid, and of high volume. Fever generally occurs in the 100°F to 102°F (38°C to 39°C) range. Vomiting is less common than diarrhea. Headaches, myalgias (muscle pain), and arthralgias (joint pain) are often reported as well.Whereas the diarrhea typically lasts 24 to 72 hours, patients often report fatigue and other nonspecific symptoms lasting 7 days or longer. For the full article: http://www.about-salmonella.com/salmonella_symptoms_risks
More discussions about infection
Source

Leave a Reply